
Osteomyelitis: Diagnostic Clues from a Clinician
Part 2
Last month, we discussed the simple clinical diagnosis of osteomyelitis – if there can really be such a thing for this often misdiagnosed complication. I suppose the most important thing in making the diagnosis is to have a high degree of clinical suspicion for it, especially in long standing or deep ulcers. As I’ve stated before, those wounds that do not heal despite good basic wound care for a period of time (at least 4 weeks) are failing to heal because there is an underlying problem. Two of the most common (and important) underlying complications in this regard would be ischemia or infection (or both). Presuming that we have ruled out the presence of ischemia, one must always consider that underlying osteomyelitis might be the reason that a chronic ulcer remains chronic and is recalcitrant to good standard care (debridement, offloading, glucose control, topical therapeutic agents, etc.). As discussed in the previous issue of Foot Notes, the probe to bone (PTB) test might be your easiest way to assess for bone involvement (if the PTB test is positive, I would consider it highly likely that clinical osteomyelitis or osteitis is present). Since plain film radiographs are notoriously insensitive for acute and sometimes chronic osteomyelitis, a negative X-ray cannot lull us into thinking that osteomyelitis is not present when there are no visible radiographic changes. As much as PTB negative ulcers can have negative X-rays, so too can PTB positive ulcers. Nonetheless, in both circumstances true osteomyelitis can indeed be present. This is the clinical conundrum that we all face when examining our patients and it is exactly the reason why we need to have a high index of suspicion for osteomyelitis. Simply stated, if you look for it, you will find it.
Of course, when there are radiographic osseous erosions under the base of an ulcer, we can usually make the diagnosis rather easily (unless Charcot arthropathy is present as well). (Figure 1) I would have to say that in my experience with patients presenting fairly early in the course of their diabetic foot ulcers (DFU), this is more the exception than the rule. Most X-rays are negative in this setting, but they still need to be performed – even to look for foreign bodies or gas (as we have discussed in our articles on diabetic foot infections). Therefore, I consider it a fairly standard part of practice to obtain foot X-rays at least at some point during the management of DFUs. This is supported by several peer reviewed guidelines and reviews on this topic. When plain film radiographs are negative for bone changes and your suspicion remains high (as it should in many cases), you will need to investigate further to ascertain the presence (or absence) of osteomyelitis.
|
Figure 1: A chronic heel ulcer with obvious erosions visible on X-ray indicative of osteomyelitis.
|
 |
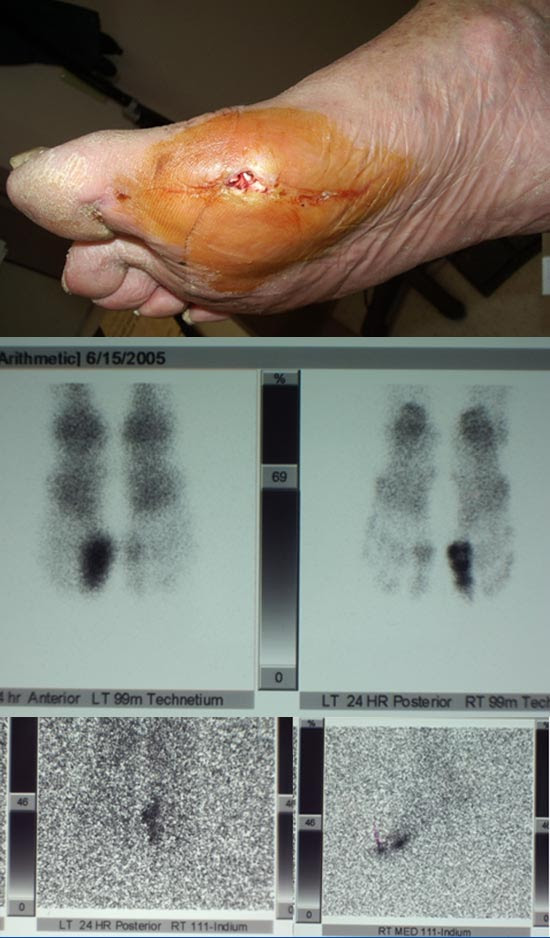
My first choice for advanced imaging in outpatients suspected of having osteomyelitis is the very common three phase technetium bone scan. While I certainly appreciate the fact that this highly sensitive test is also not specific for bone infection, I only order it when I suspect that this is indeed present. A bone scan is far easier for me to obtain than an MRI, so I am quite comfortable basing my treatment plans on this common modality. If positive, as it usually is in these circumstances, a combined bone and Indium scan is ordered. The combination of tests provides both sensitivity and specificity, since the Indium leukocyte scan is quite specific for bone infection (few false positives- except in the presence of Charcot arthropathy). I’ve rarely seen a false negative Indium scan when the disease was indeed present, but this can happen nonetheless (high negative predictive value). When the combined test is positive, I have made the diagnosis of osteomyelitis with a degree of certitude and treat accordingly. (Figure 2)
|
Figure 2 (a, b, c): Chronic osteomyelitis with positive bone scan and Indium scan in a draining wound that probes to bone and with negative plain X-rays (not shown).
|
 |
Despite my rationale above, the consensus of opinion is that MRI (with or without contrast) is the modality of choice for diagnosing osteomyelitis. Aside from being highly sensitive and fairly specific due to the superb anatomical and physiological detail provided, MRI can also help determine the extent to which the bone is infected. This is important not only for diagnosis, but also for operative planning. Consider the frequent clinical scenario of a patient with recalcitrant osteomyelitis and positive bone cultures, X-rays, and even Indium scans. An MRI can establish how much of the bone is involved and, accordingly, how much must be resected when considering surgical intervention. (Figure 3)Another situation that might arise is when osteomyelitis of an exposed metatarsal head is diagnosed, but you are concerned about adjacent metatarsal or phalangeal involvement as well. An MRI is an excellent imaging modality to evaluate such concerns. I tend to rely on MRI most frequently when we have a patient admitted with a moderate to severe diabetic foot infection (IDSA 3 or 4), a strong suspicion for osteomyelitis, and the need to ascertain areas and extent of involvement for surgical planning. Additionally, MRI is an excellent imaging modality to use when there is suspicion for an underlying abscess not fully appreciated on clinical exam (especially along tendon sheaths and fascial compartments). Unfortunately, our use of gadolinium contrast has been limited due to concerns for nephrogenic systemic fibrosis (NSF) in such patients with renal insufficiency.
|
Figure 3: Chronic heel ulcer with negative X-ray and positive MRI for osteomyelitis. No bone was exposed and probe test was inconclusive due to granulation tissue covering the bone (false negative test). A subtotal calcanectomy was recommended.
|
 |
While CT scans, diagnostic ultrasound, and especially PET/CT are also useful modalities to diagnose osteomyelitis, my clinical experience with them limits my ability to discuss them in proper context. Nonetheless, the latter is probably the most exciting modality in this regard and can combine high sensitivity, specificity, and spatial resolution. While several reviews on PET/CT for diabetic foot osteomyelitis are currently published, this modality is not yet universally available and clinical experience with it is still evolving in this regard.
Notwithstanding the accuracy of these advanced modalities in assisting with the diagnosis of osteomyelitis, we must recognize that there is no such modality with 100% accuracy. Specifically, we must always use our clinical judgment and acumen when interpreting these imaging studies.
Not all “hot” scans or positive MRIs truly represent bone infections. Beware of false positive results, especially in the presence of Charcot arthropathy or prior trauma. (Figure 4) We don’t treat X-rays (or other imaging modalities): we treat people. I’m a firm believer in putting two and two together – if the clinical picture doesn’t fit what you are seeing on imaging, go with your instincts – especially in this scenario when there is really no urgency to make a diagnosis of osteomyelitis.
|
Figure 4: X-rays in a patient with a chronic ulcer over his lateral 5th metatarsal head. X-rays demonstrate numerous changes in forefoot and midfoot and combined Bone/Indium scan suggested osteomyelitis of the 4th and 5th metatarsals. Ultimately, it was recognized that he had prior fractures in the midfoot accounting for the false positive bone and Indium scans. His ulcer only probed to the 5th MTP joint and clinical osteomyelitis was diagnosed only for that area.
|
 |
Now that we’ve discussed making the clinical diagnosis, next month we’ll discuss various treatment options for osteomyelitis that I’ve found effective over the years.
| ### |
|---|
References are provided below that can expand upon many of the points made above. We welcome your opinions, concerns, and suggestions. If you have an interesting case or a troubling circumstance that you would like to share with fellow PRESENT Diabetes members, please feel free to comment on eTalk.
Best regards,
Robert Frykberg, DPM, MPH
PRESENT Editor,
Diabetic Limb Salvage
REFERENCES
|
