Snail mucus yields natural adhesive for wound healing
by Zhang Nannan, Chinese Academy of Sciences
Land snails and their mucus were used in ancient times by Hippocrates and Pliny to treat pain associated with burns, abscesses and other wounds. Inspired by this ancient therapy, Prof. Wu Mingyi and his team at the Kunming Institute of Botany (KIB) of the Chinese Academy of Sciences identified a natural biological adhesive from snail secretions, evaluated its in vitro adhesion properties and studied its in vivo effects on wound healing.
The results have been published in Nature Communications.
Every year, hundreds of millions of people suffer from various tissue wounds, ranging from minor skin cuts to severe injuriescaused by trauma, surgical injuries or chronic ulcers. In particular, chronic wounds, such as diabetic foot ulcers (DFUs) and pressure sores. Among them, dysregulated inflammation has been identified in the process of diabetic wound healing.
In fact, proinflammatory baseline states are found in diabetic patients and animal models even before wounding. The chronic proinflammatory environment in diabetic wounds prevents progression to the proliferative phase of wound healing, and impairs key processes of tissue repair such as angiogenesis, extracellular matrix (ECM) remodeling and re-epithelialization.
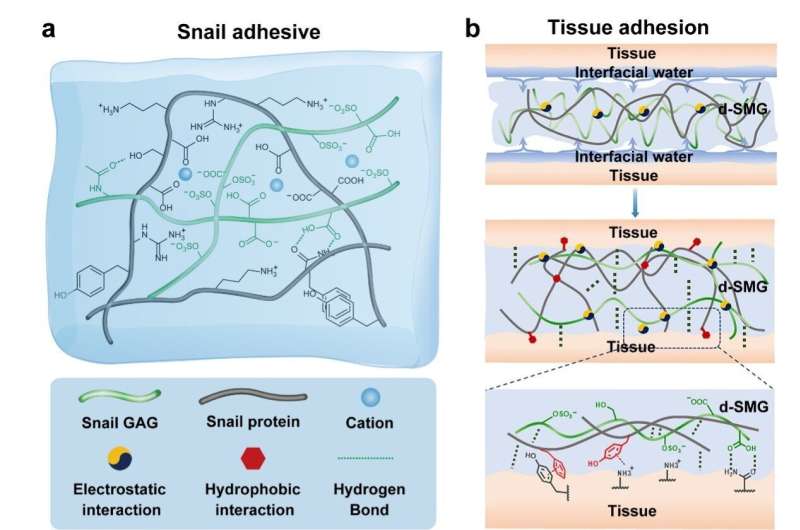
In this study, the researchers found that the natural biomaterial (d-SMG) consists of 30%–50% protein and 10%–16% sulfated glycosaminoglycan (GAG). The composition of d-SMG is similar to that of ECM which is composed of fibrous proteins and polysaccharides, and provides mechanical support for cell growth and regulates cell behavior.
d-SMG exhibited better adhesion performance in wet tissue than the clinical fibrin glue in both vitro and vivo studies. The natural GAG-protein-based gel provides a moist tissue micro environment with reduced inflammation that is in favor of tissue regeneration.
In vivo study showed that d-SMG promoted skin wound healing in both normal and diabetic rat models. It improved the angiogenesis, granulation tissue neogenesis, collagen deposition, and epidermal regeneration in the wound bed.
For diabetic wounds, the mechanism study showed that both d-SMG dressing and its active ingredient s-GAG promoted the polarization of macrophages towards the anti-inflammatory M2 phenotype by upregulating STAT3 phosphorylation, which may contribute to the transition of wound healing process from inflammation to proliferation, thereby accelerating wound healing.
In addition, d-SMG has a high content of heparin-like GAG, which can also bind the inflammatory cytokines (TNF-α, IL-6, IL-8, and IP-10) with high affinity.
As a result, d-SMG reduced the levels of inflammatory cytokines (TNF-α, IFN-γ and IL-6) in wound tissues possibly by both regulating macrophage polarization and capturing inflammatory cytokines.
The researchers found that a natural glycosaminoglycan-based snail mucus gel can seal skin wounds and promote diabetic wound healing.
These findings provide theoretical and material insights for the development of bioactive dressings and bioengineered scaffolds for wound healing.
In the future, they hope to use the bioadhesive as a novel treatment for DFUs. By targeting the pathogenesis of DFU, the researchers aim to develop more effective drugs or wound dressings for clinical use.
More information: Tuo Deng et al, A natural biological adhesive from snail mucus for wound repair, Nature Communications (2023). DOI: 10.1038/s41467-023-35907-4
Journal information: Nature Communications