|
 by Jay Lieberman DPM, FACFAS |
 |
This 54-year-old insulin dependent diabetic was initially treated for a sterile bullae on the posterior aspect of the left heel. There was no precipitating acute trauma or thermal injury.
PAST MEDICAL HISTORY: This includes hypertension, diabetes, peptic ulcer and osteoarthritis.
MEDICATIONS: Catapres, Lovenox, Insulin, Zestril, Lisinopril and Reglan.
ALLERGIES: Percocet
FAMILY HISTORY: Diabetes, history of GI bleed.
SOCIAL HISTORY: Previous history of smoking, ceased more than ten years ago.
SURGICAL HISTORY: The patient has had left toe amputation, right ankle surgery times two, cholecystectomy and trigger finger release.
Activity Level
TREATMENT AND COURSE
After two weeks, the bullae dried into a gangrenous eschar with minimal moist necrosis in the deeper layers. The eschar was loosely adhered to the heel. The patient was seen weekly for debridement of devitalized tissue.
A L’Nard splint was utilized to offload the area. Home healthcare did daily assessments and applied enzymatic debridement agents with dressing changes.
This patient slowly developed a poor quality granulating base. Although there was some evidence of improvement, new areas of necrosis were seen. After some time, a component of the Achilles tendon could be visualized. Her pain level was between a 5 or 6 out of 10, giving a high suspicion that ischemia was a larger component of the problem than originally thought.
The patient was sent for a vascular evaluation. Peripheral flow to her leg was marginal at best. Stent placement would be considered, only if the wound would not heal, as patient was not an ideal candidate for surgical intervention. The arterial Doppler suggested partial occlusion of the femoral artery with calcifications in the distal branches.
Two months after the initial presentation, the patient came to the office with large bullae formation along the medial and lateral walls of the calcaneus.
 |
 |
 |
|
|
Infectious Bullae Medial Wall
(post debridement) |
Bullae Lateral Wall (post debridement)
|
Moist necrosis Heel with MRSA
|
Erythema, fluctulance and drainage were readily apparent. Cellulitis and lymphangitis were noted. Cultures taken at that time indicated a MRSA infection.
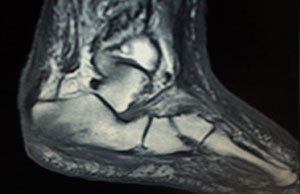
| The patient was admitted to the hospital and started on Vancomycin. An MRI indicated marrow signal changes in the posterior calcaneus compatible with osteomyelitis. | Standard x-rays showed loss of normal cortical structure. | |
 |
 |
|
| MRI | Standard Radiograph |
Hospital Admission
Upon admission, the patient’s WBC was 22, 000. Blood glucose was 360. Blood cultures were negative. After 48 hours, a partial calcanectomy was performed with wound debridement.
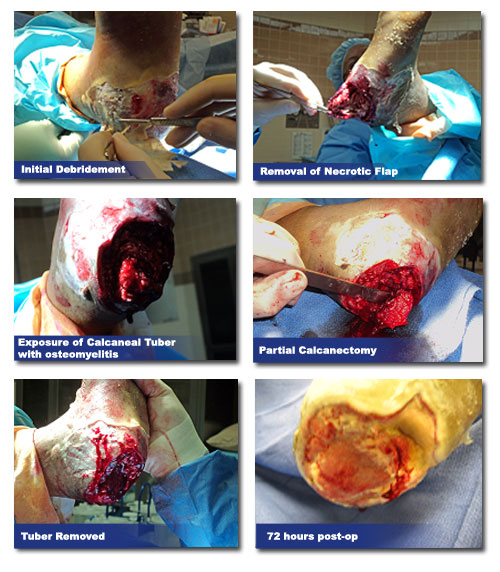
Postoperatively negative pressure wound therapy was initiated.
 |
 |
|
|
VAC in place
|
||
2nd Hospital Admission
During a subsequent hospitalization, stents were placed in the left leg. The quality of the granular bed improved markedly over the next two to three weeks.
Ultimately, a GRAFTJACKET® t was applied to the heel to further promote healing. Below is the most recent photograph showing the patient at one month status post surgery.
 |
 |
 |
| GRAFTJACKET® Applied |
GRAFTJACKET® from KCI
|
One month post-op |
 |
 |
|
|
Two month post-op
|
10 weeks post-op
|
At this point the options available to us are:
- Hyperbaric Oxygen Therapy to promote further neovascularization
- Debridement of undermined tissue with second application of synthetic skin
- Debridement of undermined tissue with direct application of split thickness skin graft
- Application of silver dressing to decrease bacterial load